Perspectives
Predictive modeling: building the foundation for savings and protection, Part 3
Insights+ -- finds savings opportunities; PreserveRx – provides protection from financial risks
March 5, 2021This three-part series looks at drug super spenders: Part 1 looks at who these members are. And why integrated data is so crucial to understanding their health care needs and health care costs. Part 2 examines why this group of members is growing so fast. It looks at Prime’s effective use of pipeline management and value-based contracting. Part 3 looks at solutions that can support health outcomes and save millions of dollars on high-cost drugs.
Prime’s research gets put to work at the member level, at the plan level, and across our book of business. It’s designed that way. We call that actionable analytics. And it starts with the member. Because what’s good for the member is good for all of us. Health care solutions need to work for all of us.
Insights+ can give a health plan the big picture of one patient’s total drug therapy
Changing from tablets to capsules saved $90,000 for one patient. A patient was prescribed Imbruvica® (ibrutinib) tablets. This is a targeted therapy for treating cancer. As a result of the manufacturer’s pricing strategy, ibrutinib tablets cost more than the same dosage of ibrutinib capsules.
Insights+ is Prime’s web-based platform with artificial intelligence and access to our integrated medical and pharmacy claims data. It helped identify that the patient taking the higher priced tablet form could be taking a formulation of the drug in a lower-priced capsule.
The $12,000 monthly charge for the tablet form of Imbruvica was in sharp contrast to the $4,000 monthly charge for the capsules for the same dosage (140mg). That added up to $90,000 for one year for one patient.
The plan had around 100 patients on Imbruvica. There might only be a few patients of them on tablets instead of capsules. But Insights+ can easily find those needles in the haystack. Then we could figure out how they got through current utilization management (UM) strategies and provide feedback upstream to make the safety net stronger.
This discovery led to the creation of an upstream UM strategy that could save Blue Plan clients millions of dollars a year. The Blue Plan also reached out to ask providers to switch any current patients taking tablets to the capsule form.
Applying Insights+ at a plan level grows its impact significantly
Our goal is to help members improve their health while also saving money. We’ve shown our Blue Plan clients how to use a specially trained managed care pharmacist to review the claims of high drug-cost member files. Several of our health plan clients have reported significant results in this way.
 This program demonstrates the importance of providing managed care pharmacists with appropriate access to data. That way they can help make sure that high-cost specialty therapies are used safely and cost-effectively, regardless of benefit.
This program demonstrates the importance of providing managed care pharmacists with appropriate access to data. That way they can help make sure that high-cost specialty therapies are used safely and cost-effectively, regardless of benefit.
One plan, with 1.5 million members, assigned one managed care pharmacist to review high-drug cost members’ drug therapies.
Over the course of one year, the pharmacist focused on comparing prior authorization approvals to claims dispensing patterns. With Insights+, medical and pharmacy claims were available for examination.
The pharmacist identified a range of high impact opportunities that ultimately saved the plan $2.7 million. The pharmacist, in collaboration with the BCBS plan pharmacy department, executed on the following savings opportunities:
- The hepatitis C PA detailing process was improved so that only 56 days of therapy was dispensed. This resulted in more than $1 million in savings.
- A fraud, waste and abuse (FWA) investigation of a pharmacy found suspicious dispensing patterns of high-cost claims. This resulted in nearly $700,000 of savings.
- One patient was over-using acute drugs for hereditary angioedema, using two acute drugs where one is recommended. A consultation with the patient’s doctor resulted in selecting one acute drug (ending the other prescription). Focusing efforts on dosing modifications with one prescription was more successful. This saved the plan more than $462,000.
- Dosing can be a challenge for some of these high-cost drugs. With dosing review and optimization, savings quickly added up. This affected:
- Nine members on secukinumab for a savings of more than $327,000
- One member on selexipag for a savings of $71,000
- One member on adalimumab for a savings of $56,000
- One member on ibrutinib for a savings of $31,000
- Seven members on a range of other drugs for a savings of $29,000
The grand total came to $2.7 million in savings.¹ The personnel investment for one pharmacist balanced against the direct savings gave a return on investment of 9:1 for one year’s effort.
Applying Prime’s significant clinical knowledge to predictive modeling
Prime’s use of predictive modeling has been honed by years of use in ³ for the traditional drug categories (adherence, controlled substance use and abuse and others). Based on our groundbreaking research, predictive modeling is now also built into the products that target the narrow band of drug super spenders.² ³
Insights+ works into the future
Insights+ can provide a High Cost Predictive Model report that will show plans how to target interventions on members that are likely to become drug super spenders within 12 months. These members are not super spenders yet — but based on known patterns, we think they probably will be.
For example, we’ve found that members are likely to become a super spender if they are, for example, on a targeted drug list, or have total drug costs on the pharmacy benefit and medical drug costs on the medical benefit in the previous 12 months above a certain level.
Our report provides:
- Prediction of whether the member will spend greater than $250,000 in medical and pharmacy drug claim expenditures during the next 12 months
- Probability that the member will have over $250,000 in medical and pharmacy drug claim expenditures in the next 12 months
The report also predicts the total drug spend the member will have in the next 12 months and if they are expected to have an increase or decrease in their drug expenditures.
The report lists and prioritizes possible interventions. It also provides direction for those interventions, such as duplicate therapy, site of care, and more.
Predictive modeling shows us where there are significant savings opportunities, if we act now.
Protecting access to life-changing gene therapy — PreserveRx
We all want access to potentially life-changing or curative gene therapies. But the costs for these ultra-expensive therapies can be prohibitive.
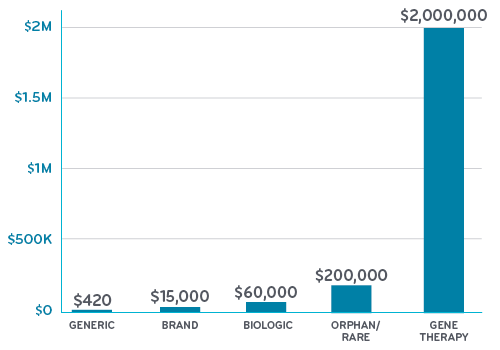
We’ve been complaining about rising costs of brand drugs for several years. Well, the costs for orphan drugs and gene therapy go far beyond the pricing of brand and generics. Where a generic might cost $420 a year, an orphan drug might cost $200,000 or $400,000. And gene therapy costs can be in the millions.
Average annual price per drug category
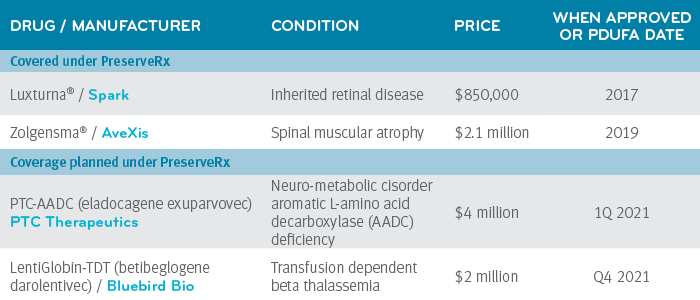
 PreserveRx is a clinical and financial solution designed to reinsure high-cost gene therapies, specifically for Blue Cross and Blue Shield Plans. It protects payers from sudden, one-time costs due to covering ultra-expensive gene therapies. It’s offered by Prime, together with BCS Insurance Company, and is designed to help payers cover these gene therapies and therefore help preserve member access and coverage.
PreserveRx is a clinical and financial solution designed to reinsure high-cost gene therapies, specifically for Blue Cross and Blue Shield Plans. It protects payers from sudden, one-time costs due to covering ultra-expensive gene therapies. It’s offered by Prime, together with BCS Insurance Company, and is designed to help payers cover these gene therapies and therefore help preserve member access and coverage.
Drugs covered or planned under PreserveRx
PreserveRx has a financial component to provide payer relief associated with one of the covered gene therapies. Its clinical services component forecasts financial impact and potential use, leveraging:
- Integrated medical and pharmacy claims data
- Clinical research
- Expert analysis
PreserveRx reduces the financial risk to high-cost gene therapies for therapies currently available and select new products as approved.
PreserveRx provides access to savings through outcomes-based contracts that track and report member outcomes over many years. These contracts provide the evidence that the therapy works as designed.
Prime’s research to identify the number of drug super spenders provided the foundational insights to inform the development of PreserveRx.
Don’t wait to get ahead of the growth of drug super spenders
This series of articles has shown the growing impact of drug super spenders on drug spend. It’s provided context for that growth and presented some of Prime’s strategies for managing this spend. With programs informed by data analytics, Prime can work with its Blue Plan clients to help optimize health outcomes and control costs for drug super spenders.
References
- Hintze P, Dauer S, Eckwright D, Gleason P. Specialty Drug Managed Care Pharmacist Clinical Review Program Savings Among 1.5 Million Commercially Insured Lives. Academy of Managed Care Pharmacy: Virtual meeting April 2020. J Manag Care Spec Pharm 2020;26(4-a):S72. https://plan.core-apps.com/amcp2020/abstract/a952fc2ad5de2fbd1164d14c6bd30739
- Bowen K, Gleason P. Drug Super Spenders:2016-2018 Growth in Number of Members and Total Pharmacy Plus Medical Benefit Drug Cost for Members with Extremely High Annual Drug Cost in a 17 Million Member Commercially Insured Population. Academy of Managed Care Pharmacy national meeting Baltimore, MD. October 2019. J Manag Care Spec Pharm 2019:25(10-a):S90. https://www.jmcp.org/doi/pdf/10.18553/jmcp.2019.25.10-a.s1
- Bowen K, Starner C, Gleason P. 2016 to 2019 Trend in Integrated Total Pharmacy Plus Medical Benefit Drug Spend—Doubling of Members with Extremely High Annual Drug Cost within a 17 Million Commercially Insured Population. Academy of Managed Care Pharmacy virtual national conference. October 2020. Accessed at: https://www.primetherapeutics.com/content/dam/corporate/Documents/Newsroom/Pressreleases/2019/document-amcpposter-superspenders.pdf
Drug names are the property of their respective owners.
Related news
Perspectives
April 25, 2024
Clinical News: April 2024
Your monthly source for drug information highlights
Perspectives
April 25, 2024
Drug Approvals Monthly Update: April 2024
This monthly update of United States (U.S.) Food and Drug Administration (FDA) approvals…
Perspectives
April 24, 2024
Prime/MRx resident wins AMCP Foundation Best Poster Award
Ai Quynh Nguyen, PharmD, was recently recognized for her research on opioid-prescribing patterns and outcomes