Perspectives
When adherence goes higher, associated medical costs go lower
For costs, good adherence is good, and better adherence is even better.
December 21, 2020Research has established that adherence to medication therapy – taking medications as prescribed – is associated with lower health care costs.¹ ² For Medicare Star rating categories, adherence of at least 80 percent of days covered (>80 PDC) has been the standard to reach.
Now we’re finding that adherence higher than 80 percent is potentially even better. Higher adherence can be associated with even greater cost reductions. We didn’t know that until we dug deeper into the data.
 With health care costs growing, efforts to improve adherence need to focus where those efforts are associated with lower use of resources and a lower cost of care.
With health care costs growing, efforts to improve adherence need to focus where those efforts are associated with lower use of resources and a lower cost of care.
It’s generally accepted that on balance, people don’t follow their treatment plans about half the time. A 50 percent adherence rate is very common.³ Why so low? Patients may not take their medicine as directed due to a host of reasons including perceived or real adverse effects, lack of perceived benefit, cost, convenience, or confusion. And we know that poor adherence is associated with an increased risk of hospitalization, decreased health care outcomes and increased overall health care costs.1,2 The bottom line is that poor adherence is expensive.
The percentage of days covered (PDC) is the most commonly used measure for adherence. According to the Pharmacy Quality Alliance, there is clinical evidence for a standard PDC threshold of 80 percent.4 Above that, most medications have a reasonable likelihood of achieving clinical benefit. That becomes the measure of success.
Why do we look for these standard adherence rates?
Having more members who take medicines as prescribed helps increase a health plan’s Star rating. A higher Star rating helps plans attract new members and earn Centers for Medicare & Medicaid Services (CMS) incentive payments for quality performance.
Prime and its health plan clients are rated annually based on Medicare member adherence statistics in three therapeutic categories:
- High blood pressure
- High cholesterol
- Diabetes
But there is little objective data quantifying the relationship between members’ adherence and total cost of care (TCC) or the use of medical resources.
That’s probably because most health plans can’t (or don’t) provide it. Most only provide pharmacy reports with any medical data separately, if at all.
But Prime has fully integrated medical and pharmacy data on this population. It makes a big difference. Prime’s adherence study goes beyond what CMS currently expects. We provide a comprehensive, real-world view of medication use and value.
Why are Star Ratings such a big deal?
Star ratings are an incentive for health plans to reach higher ratings that can help them attract new members and retain current members. The high ratings also come with important financial benefits that help fund improved programs.5 Increasing a Star rating is a tasty carrot because of the big money that comes with it. This year, the incentive payments earned are worth hundreds of millions of dollars. Our health plan clients will use them to create or enhance programs that serve their Medicare members.
A major study of Medicare members6
Prime conducted a study of 20 Medicare Advantage contracts with its members receiving pharmacy benefits from Prime. We looked at two years, from January 2017 to December 2018. We analyzed and sorted the population for specific eligibility criteria.
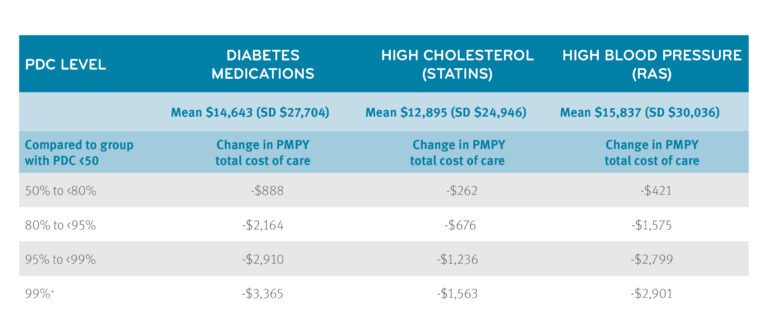
Associated total cost of care savings got bigger with every increase in adherence
The study showed that moving someone with low adherence (<50%) to near perfect adherence (99%+) was associated with potential total cost of care savings, as follows:
- High blood pressure drugs (renin angiotensin system agents or RAS) were associated with $2,901 potential savings per person per year (PPPY)
- High cholesterol (statins) were associated with $1,563 potential savings PPPY
- Diabetes medications were associated with $3,365 potential savings PPPY
Plus, each one PDC percentage point adherence increase was associated with a cost-of-care decrease of $21 to $46. The specific cost decrease varied by category.
Additionally, the study found improved drug category adherence was associated with fewer medical events, including hospitalizations and emergency room visits. Less time in the ER and hospital means better quality of life. More information on that can be found in the research poster.6 This research won a silver award from the Academy of Managed Care Pharmacy (AMCP) at its Nexus 2020 virtual event in October 2020.
People who are more adherent are probably more aware of their health in other ways
We must remain mindful that these results cannot be separated from what is called the health adherer effect: members who are health conscious in other aspects of their lives may more likely to be adherent to drug therapy.7
What made us want to look at adherence rates higher than 80 percent?
CMS can update its requirements for Star ratings every year. We’re constantly looking for new ways to be one step ahead, so we’re ready for new CMS requirements. Plus, our data on adherence teaches us more about Medicare members as patients and as consumers of health services. We learn, develop new ideas, and invest more resources in the programs that work. Each program improvement helps us better serve our members and achieve better health outcomes.
Making this information work for our health plan clients
 We have a robust portfolio of products that support adherence for Medicare and commercial audiences (see the appendix). This research also:
We have a robust portfolio of products that support adherence for Medicare and commercial audiences (see the appendix). This research also:
-
-
-
- Helps us further refine our predictive modeling for several of these programs
- Gives us associated cost-of-care ROI information that may encourage broader use of these programs
- Incentivizes the development of new programming that pushes for higher levels of adherence
-
-
This (and other) research prepares us well for next year’s Star ratings evaluation. We are prepared even before we get the Medicare Advantage and Part D Rate Announcement and Final Call Letter from CMS. We always want to be ready to help our Medicare clients achieve the highest level of Star ratings possible. That it might be a moving target is okay by us. Together we’ll move toward better health outcomes for Medicare members.
Appendix A
Prime programs that help improve adherence
- GuidedHealth – Smart Adherence, identifies Medicare members at risk for non-adherence, and aligns them to clinical outreach services
- GuidedHealth Missed Refill campaigns and quarterly adherence outreach via mail, email, phone, text and secure message on MyPrime.com
- Prior authorization auto-renewal on select maintenance medications
- Clinical messaging to prescribers via electronic medical records (EMRs)
- Proactive outreach to prescribers and members in advance of expiring prior authorizations to avoid potential delays in therapy
- Outreach to members, encouraging them to move from 30-day to 90-day supply of medications
- Quality-based networks that provide incentives for pharmacies demonstrating high levels of medication adherence Stars formulary, designed to lower member cost share on drugs impacting Medicare Star ratings for Medicare clients Data and reporting that monitors members’ medication adherence
References
- Sokol MC, et al. Impact of medication adherence on hospitalization risk and healthcare cost. Medical Care. 2005;43:521–530.
- Roebuck MC, et al. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Affairs. 2011;30:91–99.
- PQA Adherence Measures. August 18, 2018. © Copyright 2018 Pharmacy Quality Alliance Accessed November 22, 2020: https://www.pqaalliance.org/adherence-measures
- ” Cost of Not Taking Your Medicine,” by Jane Brody. April 17, 2017. New York Times. © 2020 The New York Times Company. Accessed at: https://www.nytimes.com/2017/04/17/well/the-cost-of-not-taking-your-medicine.html ?
- 21 Prime Medicare contracts earn quality bonuses, October 26, 2020. Prime Therapeutics. Accessed at: https://www.primetherapeutics.com/en/news/Stories/2020/story-21-Medicare-Earn-4-Star-Ratings.html
- Is Medicare Star Category Medication Adherence Associated with Lower Total Cost of Care and Medical Events? By Y. Qiu, MS, Karaca Mandic, PhD, Gleason, PharmD, Prime Therapeutics, LLC, Eagan, MN,; Accessed at: https://www.primetherapeutics.com/content/dam/corporate/Documents/Newsroom/Pressreleases/2020/document-2020-amcp-adherence.pdf 7. Healthy adherer effect – the pitfall in the interpretation of the effect of medication adherence on health outcomes. J Eval Clin Pract. 2014;20(2):111- 116. https://onlinelibrary.wiley.com/doi/abs/10.1111/ jep.12095.
Related news
Perspectives
July 25, 2024
Quarterly Drug Pipeline: July 2024
Clinical insights and competitive intelligence on anticipated drugs in development
Perspectives
July 22, 2024
Oncology Insights: 2024 ASCO Annual Meeting key findings
Findings from this year’s American Society of Clinical Oncology (ASCO) Annual Meeting will likely lead to clinical practice changes and U.S. Food and Drug Administration (FDA) drug approvals or expansions
Perspectives
July 16, 2024
LISTEN NOW: Beyond the business – Stories of corporate kindness | Pharmacy Friends Podcast
In this episode, we talk about how our employees' help goes beyond our work in health care, aiding in philanthropic efforts