PerspectivesStories,
Teaching our members with diabetes how to juggle
Because most people with diabetes have other conditions as well.
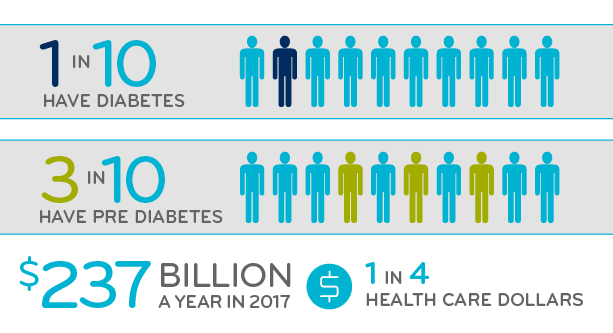
March 5, 2019It’s big. Over 30 million children and adults in the United States have diabetes. Every year, another 1.5 million Americans get a new diagnosis of diabetes.1
It’s expensive. Nationally, diabetes cost $237 billion in 2017 – 1 out of every 4 health care dollars.2
It’s complicated. People with diabetes have a lot of related conditions like cardiovascular disease, heart attacks, strokes and kidney disease. They manage glucose levels plus blood pressure and cholesterol levels to prevent these related conditions. The American Diabetes Association publishes an online 172-page Standards of Care for Diabetes. It’s updated not just annually, but all year long.3
We get it. Diabetes is a big, expensive, complicated disease.
 Picking the right drug. Taking the right drug consistently. Sounds easy in theory.
Picking the right drug. Taking the right drug consistently. Sounds easy in theory.
Our most recent study on diabetes looked at members newly diagnosed with diabetes who also had pre-existing cardiovascular disease (ASCVD). Two big findings stand out:4
Drug selection: Nearly one third of these members were not prescribed the specific drugs clinically shown to give them the best chance of preventing cardiovascular events.
Adherence: About half of the members in the study had stopped taking their add-on drug therapy within a year.
Drug selection for one third did not align with standard of care
Three separate antihyperglycemic drug classes provide add-on therapy for people with diabetes who also have ASCVD. The American Diabetes Association (ADA) recommends trial of the first and second drug classes, before going on to try the third drug class. These guidelines, which have been proven to be both clinically and cost effective, recommend the following order of therapy:
- Glucagon like peptide-1 agonists (GLP-1)
- Sodium-glucose cotransporter-2 inhibitors (SGLT-2i
After trial of 1 and/or 2, (step therapy) then try:
3. Dipeptidyl peptidase-4 inhibitors (DPP-4i)
In our study of 44,021 commercial members, nearly one third (14,028) had a first antihyperglycemic claim of DPP-4i. Yet according to the guidelines, these 14,028 members should have first had a trial of a GLP-1 and/or a SGLT-2i before being prescribed a DDP-4i.
Add-on antihyperglycemic therapy for people with diabetes who also have ASCVD

Over the four years of this study, the percentage of members starting a DPP-4i before a GLP-1 or SGLT-2i did not decline. This, despite:
- Publication of clinical trial results
- FDA approved labeling use of a GLP-1 or SGLT-2i for ASCVD
- Professional guidelines’ recommendation for use of GLP-1 or SGLT-2i in this subset of patients (when lifestyle management plus metformin does not achieve or maintain A1C goal)
In summary, one-third of members prescribed an antihyperglycemic were not prescribed the first- or second-line therapy. And this percentage did not improve over the course of four years, despite higher visibility of this standard of care.
Adherence to therapy for all three of these drug classes was an issue
About half of the members taking these medications discontinued within one year. (Yet the drug manufacturers reported adherence of 90 percent in their clinical trials.)
All these medications require long-term adherence to reduce complications from ASCVD. But for all the drug classes in the study, adherence dropped off by about half within a year.
What can we do?
Small changes in drug therapy management can make a difference. Several strategies can support drug selection along clinical guidelines:
- Utilization management programs, like prior authorization or step therapy
Preferred drugs in the formulary, supported with benefit design
This drop-off in adherence suggests the potential for value-based contracting with manufacturers. Value-based contracting can encourage accountability by focusing on quality of care. It aligns payers, members and providers by focusing on improved health outcomes. In addition, adherence interventions can target members at risk and/or their providers.
Juggling the complex care of members with diabetes
“Juggling” is a synonym for “managing.” Whether from a member or a plan perspective, it’s a fitting description for dealing with diabetes. It’s a tricky coordination act, keeping several pieces moving, just the right amount at just the right times.
If managed care can help with benefit design or cost share or UM, it makes it just a little easier for the member with diabetes to manage everything else.
References
- http://www.diabetes.org/diabetes-basics/statistics/
- Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care March 2018. American Diabetes Association. Accessed at: http://care.diabetesjournals.org/content/diacare/early/2018/03/20/dci18-0007.full.pdf
- Standards of Medical Care Diabetes – 2018. The Journal of Clinical and Applied Research and Education. Volume 41 | Supplement 1. American Diabetes Association. Accessed at: http://care.diabetesjournals.org/content/diacare/suppl/2017/12/08/41.Supplement_1.DC1/DC_41_S1_Combined.pdf
- Bowen K, Gleason P.P. “Among Commercially Insured Members with Diabetes Mellitus (DM), Choice and Persistence of Drug therapy: Dipeptidyl peptidase-4 inhibitors (DPP-4i) Versus Glucagon like peptide-1 agonists (GLP-1) or Sodium-glucose cotransporter-2 inhibitors (SGLT-2i).” Academy of Managed Care Pharmacy. Oct. 2018. Orlando, FL. Accessed at: https://www.primetherapeutics.com/content/dam/corporate/Documents/Newsroom/Pressreleases/2018/document-amcp-diabetes.pdf
Related news
Perspectives
July 25, 2024
Quarterly Drug Pipeline: July 2024
Clinical insights and competitive intelligence on anticipated drugs in development
Stories
July 22, 2024
Introducing the latest issue of our medical and pharmacy benefit management report
The summer 2024 issue of the Magellan Rx Report provides insights on the industry’s most groundbreaking managed care solutions in some of the most complex areas of health care
Perspectives
July 22, 2024
Oncology Insights: 2024 ASCO Annual Meeting key findings
Findings from this year’s American Society of Clinical Oncology (ASCO) Annual Meeting will likely lead to clinical practice changes and U.S. Food and Drug Administration (FDA) drug approvals or expansions