Perspectives
Study finds wide variation in hemophilia factor costs
Costs for members with hemophilia can range from $1,000 to $3 million.
July 31, 2018What can we learn about members with hemophilia when treatment costs range from $1,000 to $3 million?
Treatment needs for people with hemophilia A, hemophilia B and von Willebrand’s Disease (vWD) can vary substantially. Treatment costs per member in this study ranged from less than $1,200 per year to more than $3 million per year. This foundational study looked at factor treatment costs, looking for variables to account for the extreme range. What was the study about?
For people with hemophilia, clotting factor therapies help their blood clot normally. However, up to one-third of people with hemophilia may develop an inhibitor over time. This is a kind of antibody that causes their bodies to try to destroy the clotting factor. These individuals may need to use increasing doses of different kinds of medicines to achieve the same results. They might use high-dose factor concentrates, bypassing agents or immune-tolerance induction therapy.
This study looked at the full range of products used by people with hemophilia to better understand the cost and use of other products within the total cost of care. From there we can design better disease management and cost control strategies for these individuals.
What did we learn?
In the study, Prime identified the prevalence of different clotting factor treatments and the individual cost variables.
- Individual costs for clotting factor treatments ranged significantly, from about $1,000 to $3 million annually per member. Most people treated were younger than 25.
- More than 5 percent were treated with a bypassing product. These were the highest cost members.
- Products were billed through both the medical and pharmacy benefit. But clotting factor utilization analyzed in the medical data was less accurate than that analyzed in the pharmacy benefit. Most factor claims billed through the medical benefit do not correctly count the factor units dispensed – or even whether the product was used.
Methods
Prime evaluated 10 million commercially insured members younger than 65 and insured by 11 health plans. To be included, members needed to be continuously enrolled in 2012. We looked for medical and pharmacy data for factor and/or bypassing product claims. This narrowed the final study group down to 382 members (5 per 100,000) who were being treated for hemophilia A, B, or von Willebrand.
Results
The factor products are processed on both the medical and the pharmacy benefit. Only with integrated medical and pharmacy claims data can you understand patterns of use.
Members younger than 25 (9 per 100,000) have a significantly higher prevalence of the treatment than those older, age 25-64 (2.5 per 100,000). This difference may be due to decreased life expectancy with hemophilia and movement of these individuals out of commercial and onto Medicare or Medicaid.
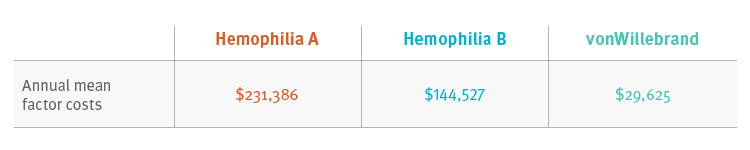
The study charts the use of factor product use by age, cost and subtype: hemophilia A, hemophilia B and vonWillebrand.
Conclusions
Individual factor costs ranged widely.
Three percent (13) members had a bypassing product claim. Seven of those members had costs greater than $1 million. Use of bypassing factor is associated with the potential to have factor costs greater than $1 million.
Factor claims are processed through both the medical and the pharmacy benefits. Claims that go through the medical benefit show less information than pharmacy claims. For example, medical claims don’t include information about member adherence, because the days’ supply is not recorded making the dosing interval hard to determine. In addition, medical claims frequently have incorrect information about the amount of factor.
What does this mean for you?
Prime recommends that all factor products be billed through the pharmacy benefit to better manage factor use. An increasing number of plan sponsors are choosing to shift coverage of factor products to the pharmacy benefit. We applaud this and encourage more of it.
Cost variation among hemophilia and vWD treatments can be attributed to the member’s diagnosis, age and use of bypassing products. Moving factor products to the pharmacy benefit will help plan sponsors better manage the use of factor products. Using a specialty pharmacy results in better information to ensure proper factor dosing, and amounts are dispensed by checking body weight, disease severity, treatment protocol and adherence. Specialty pharmacies routinely use the information on pharmacy claims to provide optimal care.
Related news
Perspectives
July 25, 2024
Quarterly Drug Pipeline: July 2024
Clinical insights and competitive intelligence on anticipated drugs in development
Perspectives
July 22, 2024
Oncology Insights: 2024 ASCO Annual Meeting key findings
Findings from this year’s American Society of Clinical Oncology (ASCO) Annual Meeting will likely lead to clinical practice changes and U.S. Food and Drug Administration (FDA) drug approvals or expansions
Perspectives
July 16, 2024
LISTEN NOW: Beyond the business – Stories of corporate kindness | Pharmacy Friends Podcast
In this episode, we talk about how our employees' help goes beyond our work in health care, aiding in philanthropic efforts