Perspectives
Prime’s missed refill program is a hit with Medicare plans
A two-touch rapid response program is the nudge members seem to need
September 7, 2018Three years ago, we turned our Medicare adherence program upside down.
The old way? We sent quarterly letters to members or their doctors with general adherence messages. It was efficient, and it was the industry standard.
Now? Upside down. Completely centered on what’s happening in the member’s life. Let’s take your mom, for example.
Day 1: Your mom runs out of the statin medication she takes for her high cholesterol. She’s got other pills she takes. Maybe she doesn’t notice that one was missing.
Day 7: Her name pops up on a report at Prime. This prescription is overdue to refill.
Day 10-13: Mom gets an automatic call: a personal message reminding her to refill that includes the name of the medication.
Day 13-15: If her refill claim does not come through within two weeks, then we send a personalized letter to your mom, first class. It includes the name of the drug she may have forgotten to refill and it offers help getting it refilled. The letter also suggests that if she gets a 90-day supply, she might save money. 90-day supplies make it easier for her to keep enough of her medication on hand.
The results of the new program were great. We tested it with one plan in April of 2015. The health outcomes team tracked the results. Prime presented the results of this study at the Pharmacy Quality Alliance (PQA) Annual Meeting May 16-18 in Baltimore.
The outreach program focused on the three Star Rated drug categories: high cholesterol, high blood pressure and diabetes. Medication refills increased 1.5 percentage points and showed an 8 percent higher refill rate among members who received the two-touch intervention compared to those who did not.
Rate of Change Intervention vs Controls
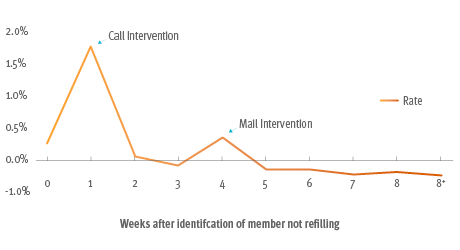
1. Rate change of the difference in percentage refilled between the intervention and control group for first 8 weeks; weeks 9, 10, and after 10 weeks (70 days) the member was considered to not have refilled.
The missed refill program delivered a statistically significant 1 to 2 percent increase in adherence for the three combined Star drug categories. And at the end of the year, those members held on to an improved adherence rate. (Members that got a 90-day supply fill had 20 percent better adherence than members that did not have a refill.)
We call the program GuidedHealth Missed Refill. Within a short period of time, all our GP clients adopted this as a plan option. From pilot to system-wide adoption – two and a half years. That’s amazing.
Timing makes a difference
The previous adherence program collected member data for a quarter before sending letters. Depending on when a member’s prescription ran out, it could be two or three months after that before the member got a letter. By that time, the member could be thinking, “What? What prescription?”
The rapid response approach works much better. And clients responded to the research. They could see the science behind the importance of early intervention and interventions timed as close as possible to the date a member’s prescription runs out.
Our standards were high
Meeting CMS standards was only table stakes. Beyond that, it took creativity and commitment to bring the right players together to make this program happen. We work closely with each of our Blue Plans. That’s important to them.
Half of Medicare members have high cholesterol, high blood pressure or diabetes. At any given point in time, 20 percent of Medicare members are nonadherent to an important treatment making rapid intervention vital to improving quality of care. Finding new ways to improve adherence is important and exciting. Finding a repeatable model that can improve refill rates and adherence can improve the Star Ratings of our Blue Plans.
Impact of the 2016 Missed Refill Intervention Program on Medication Refill Rate and 2016 CMS Star Adherence for Medicare Populations (Spring 2018)
Related news
Perspectives
July 25, 2024
Quarterly Drug Pipeline: July 2024
Clinical insights and competitive intelligence on anticipated drugs in development
Perspectives
July 22, 2024
Oncology Insights: 2024 ASCO Annual Meeting key findings
Findings from this year’s American Society of Clinical Oncology (ASCO) Annual Meeting will likely lead to clinical practice changes and U.S. Food and Drug Administration (FDA) drug approvals or expansions
Perspectives
July 16, 2024
LISTEN NOW: Beyond the business – Stories of corporate kindness | Pharmacy Friends Podcast
In this episode, we talk about how our employees' help goes beyond our work in health care, aiding in philanthropic efforts