Perspectives
Pharmacist integration delivers Star ratings, Part 2
Blue Cross & Blue Shield of Rhode Island: This team can do anything
April 30, 2018“Agility and teamwork are our strengths,” said Michael Kolodij about the pharmacists embedded within physician practices. “My team can do anything.”
Michael, who is the manager of pharmacy programs for Blue Cross & Blue Shield of Rhode Island (BCBSRI), manages the health plan’s patient-centered pharmacy program.
Part 1 in this series describes the program and how it has saved $23 million since it began in 2014. Part 2 examines how the pharmacists working face-to-face with prescribers and patients are improving Star Ratings.
BCBSRI’s patient program began with the Medicare side of the business to take advantage of the well-defined metrics in the Star Ratings program. And the health plan changed medication therapy management (MTM) vendors at the same time. After assessing the CMS-issued plan preview, RI realized its original goals were below 5-star rate thresholds. They quickly developed an end-of-year incentive program.
Undaunted, the BCBSRI team proved to be nimble and responsive to the changes and achieved the new metrics. These results helped improve BCBSRI’s Star Rating. Since implementation, BCBSRI has had an overall rating of at least 4 Stars, achieving its highest overall rating of 4.5 Stars in 2017.
The program quickly outgrew its Medicare base and the pharmacists began to serve commercial members as well. This has paid off in a big way for patients and for BCBSRI.
Helping health care work better
Pharmacists in the program call patients who have multiple chronic conditions to review medications and help problem-solve. Addressing gaps in care can improve plan quality scores. Addressing affordability helps ensure patient access to care.
On the call with the patient, the pharmacist helps:
- Address barriers to adherence
- Avoid treatment failure/adverse events caused by drug interactions
- Mitigate effects of polypharmacy due to a fragmented healthcare system and lack of communication between specialists and primary care
- Avoid unnecessary provider visits
- Reduce emergency room visits
A partnership with the patient
The pharmacist’s focus is on the patient. Ratings aren’t everything. “We are going more for the quality outcome,” Kolodij said. “We want our members to get the most out of these services. We want them to really have the opportunity to spend time with these pharmacists.”
That means calls can take three times as long as those from a call center– but they make a difference. “Our pharmacists aren’t watching the clock or driving to a call quota.”
The pharmacists agree. “We’ve finished the review, but that doesn’t necessarily mean they’re at goal. I may still need to work on blood pressure or diabetes. And that’s all time that I’m not spending doing another review,” said Kenny Correia, a pharmacist with the program.
Longer calls, yes, but also more engagement and better results
BCBSRI’s program achieved twice the patient engagement of pharmacists in call centers or from retail pharmacies.
The program also achieved twice the provider engagement rate of pharmacists in call centers and three times the provider engagement rate of pharmacists in retail pharmacists.
Embedded pharmacist program results compared to those of retail pharmacy or call center
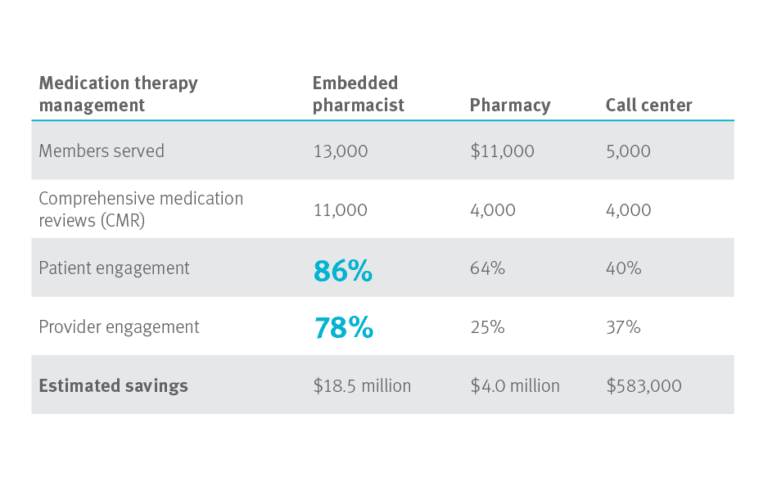 Results from 3Q2014 through 2Q2017
Results from 3Q2014 through 2Q2017
Think about integration in a new way
Prime and its Blue Plan partners are your best source of new ideas for improving health outcomes and controlling costs. Prime is working on new pharmacist outreach programs. So are other Blue Plans. The best opportunities for improved health outcomes and reduced cost of care come from integrating medical and pharmacy intelligence. We will work with plan sponsors to help identify opportunities for pharmacist-driven programs that work for you.
Related news
Perspectives
July 25, 2024
Quarterly Drug Pipeline: July 2024
Clinical insights and competitive intelligence on anticipated drugs in development
Perspectives
July 22, 2024
Oncology Insights: 2024 ASCO Annual Meeting key findings
Findings from this year’s American Society of Clinical Oncology (ASCO) Annual Meeting will likely lead to clinical practice changes and U.S. Food and Drug Administration (FDA) drug approvals or expansions
Perspectives
July 16, 2024
LISTEN NOW: Beyond the business – Stories of corporate kindness | Pharmacy Friends Podcast
In this episode, we talk about how our employees' help goes beyond our work in health care, aiding in philanthropic efforts