Perspectives
Pharmacist integration delivers big results, part 4
Blue Cross & Blue Shield of Rhode Island: Five keys to success
April 30, 2018Blue Cross and Blue Shield of Rhode Island started a patient-centered clinic-based pharmacy program in 2014 that has delivered results beyond expectations. This series explores several aspects of the program. Part 1: Complete pharmacist integration delivers results. Part 2: We’re seeing stars. Part 3: One patient. One pharmacist. Big results. Part 4: Five keys to success for a clinic-based pharmacist program
Placing pharmacists in physician practices to improve care and lower costs is a good idea. It sounds easy, right?
“I won’t lie, it was harder than we thought,” said Michael Kolodij, manager of pharmacy programs for Blue Cross & Blue Shield of Rhode Island (BCBSRI). “I’m grateful we have such a great team in place. We codified best practices as quickly as we could to capture what worked and what didn’t work. And we had a flexible and devoted team of pharmacists in the field that considered this the best job they’d ever had.”
The first three parts of this series examined how BCBSRI’s patient-centered pharmacy program works, reduced costs, improved Star Ratings and delivered dramatic results for one high-cost condition. Part 4 offers five keys to the success of a physician practice-based pharmacist program.
1. Interdisciplinary support is key. For the model to succeed, people across BCBSRI needed to buy into the program.
Clinical programs needed the executive leadership team’s (ELT) financial and program support.
ELT helped gain prescriber support for the program.
BCBSRI incorporated Star Ratings into the annual employee incentive program. This validated and reinforced the company’s commitment to the program.
2. Pharmacists have to be the right fit. Personality matters. The pharmacists need to work well with prescribers and patients. They have to be proactive in developing this role, identifying opportunities, and showing value. The program pharmacists had to demonstrate they are part of the provider team.
“Physicians are growing to really like the team approach to medicine. They worked well collaborating with me in a number of ways. I have been referred patients for a variety of reasons, such as:
- Questions/concerns about side effects
- Review of complex medication regimens
- Review of proper medication administration (e.g., proper inhaler use, glucometer use, insulin administration, etc.)
- Adherence-related concerns
- Decreasing polypharmacy (including high-risk medication use)
- OTC medication use questions” (A pharmacist in the program)
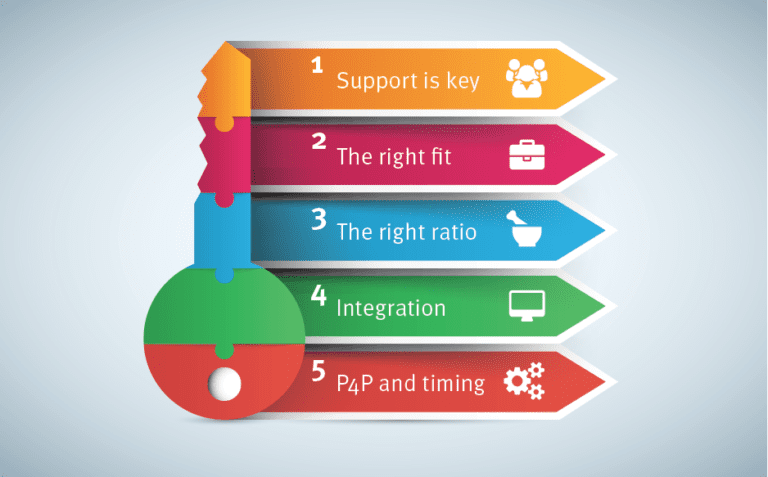 3. Find the right ratio of patients to pharmacist. Program locations have served 800 to 13,000 patients. This was an excellent testing ground to determine the right ratio of patients to pharmacist.
3. Find the right ratio of patients to pharmacist. Program locations have served 800 to 13,000 patients. This was an excellent testing ground to determine the right ratio of patients to pharmacist.
- Too small: Too few patients and the pharmacist runs through all the medication therapy opportunities and reaches all the patients before the year is over. Success rates plateau because the volume of opportunity isn’t high enough.
- Too big: Too many patients keep success rates low. The pharmacist simply doesn’t have enough hours in the day to complete all the opportunities. The program at that location would struggle to reach even a 2 Star threshold, just on volume.
- Just right: BCBSRI found that an ideal ratio of around 2,000 Medicare Advantage patients for one pharmacist provides a good balance of opportunities versus costs.
4. Take an integrated approach – looking at both medical and pharmacy measures. Integrating pharmacists into physician practices enables BCBSRI to approach patients holistically. The pharmacist can address both Medicare Part C and Part D measures. BCBSRI found that buy-in from physicians increased when the pharmacist can see the big picture, not just the drugs.
“He (the program pharmacist) has had a huge positive impact on our diabetic population. He provides diabetic teaching, suggests dosage adjustments based on sugar readings, gets patients to call in their sugar readings and sees them in office to check on their progress. He comes up with strategies to help our diabetics who cannot afford all their medicines, which is a MAJOR issue in our practice. The control of our diabetic population has definitely improved due to his efforts.”
– Robert Mathieu, MD, Internal Medicine, Providence office of Anchor Medical
5. Pay for performance (P4P) requires excellent timing. Incentive pay is tricky. It requires getting reports on time and measuring against fair expectations. Can the pharmacist impact that item? Are the expectations realistic for the opportunity? The reporting schedule must match the incentive deadlines.
Effective clinical program design must marry purposeful metrics with the infrastructure required to be successful. All departments involved must agree with the P4P approach, so they support the program with timely data.
Achoo!
Here’s an example: With the advent of pharmacist immunizers, it seemed that including the flu vaccine measure was a perfect fit for the program. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys patients to see if their providers recommended flu vaccination as a proxy for vaccination rate. What we found was that performance in a survey might not directly correlate to the actual vaccination rate. In addition, we did not have access to the member level data of who responded to the survey. So, we were not able to tie success back to specific practices. Based on these limitations, the measure was not carried forward in the program.
For BCBSRI, the program demonstrated its ability to increase engagement for patients, improve health outcomes and lower healthcare costs. The program saved $23 million in avoided health care costs (Part 1); contributed to BCBSRI’s 4.5 Star Rating (Part 2) and improved the patient experience and reduced drug costs (Part 3).
These results are getting attention from other Blue Plans.
Look on Prime Insights for other stories where pharmacist interventions have made a difference.
Related news
Perspectives
July 25, 2024
Quarterly Drug Pipeline: July 2024
Clinical insights and competitive intelligence on anticipated drugs in development
Perspectives
July 22, 2024
Oncology Insights: 2024 ASCO Annual Meeting key findings
Findings from this year’s American Society of Clinical Oncology (ASCO) Annual Meeting will likely lead to clinical practice changes and U.S. Food and Drug Administration (FDA) drug approvals or expansions
Perspectives
July 16, 2024
LISTEN NOW: Beyond the business – Stories of corporate kindness | Pharmacy Friends Podcast
In this episode, we talk about how our employees' help goes beyond our work in health care, aiding in philanthropic efforts