Perspectives
Super spenders represent a tsunami of drug spend
If you think about the rise of specialty drugs as a Category 5 hurricane, and the growth of gene therapies as an undersea earthquake, you can see the rising tsunami of drug spend looking to sweep over health care spend.
December 16, 2022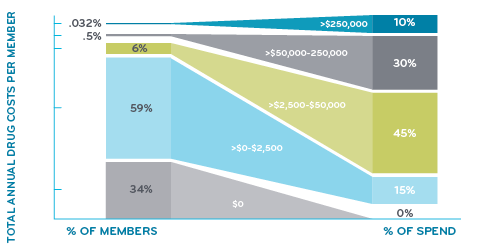
Median new drug prices for a year’s supply increased from $2,115 in 2008 to more than $180,000 in 2021.4
In 2008, 9 percent of new drugs cost $150,000 or more a year, compared to 47 percent in 2021.3 The largest price increases were in 2020 and 2021. Half of new drugs entering the market cost more than $150,000 a year in 2020 and 2021.3 And the FDA projects the approval of 11 gene therapies per year starting in 2025. Most of them have 7-figure price tags.
What conditions have drugs this expensive?
Super spenders have serious health conditions. Various forms of cancer make up nearly half of the conditions for those among drug super spenders. Inherited single gene disorders make up the next largest group. Within that group fall conditions like hemophilia A and B, cystic fibrosis, spinal muscular atrophy and hereditary angioedema. Other categories include pulmonary hypertension, multiple sclerosis and disorders treated by the drug Soliris® (eculizumab) like paroxysmal nocturnal hemoglobinuria and myasthenia gravis.
Things a PBM and health plan can do about these costs:
- Medical Policy and Utilization Management criteria applied to these drugs
- Specialty drug management
- Value-based contracting
- Pipeline monitoring
- Predictive analytics identifying future super spenders
- Super spender interventions like HighTouchRx
- Insurance and stop loss riders
Specialty drug management requires a new level of collaboration
Collaboration is needed between payers and providers for a better model that lowers total cost of care while simultaneously improving health outcomes. It’s unlikely for such collaboration to occur when there’s conflict between payer/PBMs and providers around dispensing specialty drugs.
Prime has developed an innovative new product called IntegratedRx –which brings provider-based specialty pharmacies in-network for oncology and cystic fibrosis drugs. This helps coordinate care for members and streamline the treatment process.4
In a traditional nonintegrated specialty pharmacy model, a provider has minimal connection to the central specialty pharmacy. But the new integrated program offers a connected physician, member and pharmacist experience. The channel-agnostic program makes Prime the only large PBM that doesn’t prioritize a central fill specialty pharmacy as the primary model for the member receive their oral oncolytic medications.
Value-based contracting for high-cost drugs looks at the price to value framework5
Value-based contracts (VBC) make an important contribution to controlling the costs of today’s high-cost drugs. New specialty drugs for orphan conditions often start at several hundred thousand dollars a year.
As an integrated PBM, Prime is uniquely positioned to work with drug companies to develop VBCs, aiming to improve health outcomes and lower cost of care. For example, Prime has negotiated value-based agreements with Alnylam Pharmaceuticals for two orphan drugs:
- Onpatrro® (patisiran) for the treatment of hereditary amyloid transthyretin-mediated (hATTR) amyloidosis – list price is $445,000/PMPY
- Givlaari® (givosiran) for the treatment of acute hepatic porphyria (AHP) – list price is $575,000/PMPY
Both Onpattro and Givlaari came to the market with some unknowns – related to the prevalence of the rare diseases being treated, and the alignment of real-world outcomes to those observed in clinical trials. Value-based agreements structured to address these risks may help to manage the costs of these drugs.
Even with a value-based agreement, if the initial price is higher than the drug’s price to value, there is still some negotiating to do in a value-based contract. Both Onpattro and Givlaari fall under the medical benefit. Their performance to the contract parameters will be assessed against both medical and pharmacy claims. For example, after the plan pays to treat these individuals, how does the plan ensure the treatment is working the way the manufacturer says it’s going to work? How does the manufacturer back up its product?
Prime keeps clients ahead of the drug pipeline
Our clinical and trade relations teams keep a keen eye on drugs likely to be approved by the U.S. Food and Drug Administration (FDA). Prime practices “no surprises” pipeline management with monitoring and forecasting.
Pipeline monitoring: When are these therapies coming? Who are these therapies for? What condition does it treat? What does the treatment cost? Is the treatment safe and effective?
Population estimating/risk pricing forecasting: How many patients have the condition that this therapy is designed to treat? Is it for everyone with that condition, or just certain forms of it? How many patients could a particular plan need to treat? Over what time frame? Will they all want to be treated in the first year? Once the pent-up demand is treated, what will the pace of new patients be?
Predictive modeling optimizes drug therapy6
Among commercially insured plans in a Prime study, one in 20 members with actively treated breast cancer were predicted to have more than $100,000 in drug therapy costs annually. With its successful “drug super spender” predictive model, Prime applied its predictive modeling approach integrating medical and pharmacy claims data to identify members with higher costs for breast cancer treatment. After identifying these members, they were then targeted for drug therapy optimization (for example, switching to biosimilars or other lower cost therapies).
High-cost breast cancer member indicators in the model include member demographics, financial risk scores, diagnosis codes, breast cancer type, previous spending, drug utilization, and timing of surgery relative to drug therapy. The key predictors identified included previous total drug spend in the past 12 months, use of drugs associated with HER2-positive status, metastases indicators, and hormone receptor positive or negative diagnoses.
HighTouchRx is a super spender intervention7
Prime’s clinical predictive modeling and machine learning algorithms are identifying big savings for health plans. HighTouchRx is a pharmacist to provider outreach product that utilizes Prime’s clinical predictive modeling and machine learning algorithms, which run on integrated medical and pharmacy data, to target member level drug therapy optimization and savings opportunity interventions.
From Sabril® to vigabatrin: HighTouchRx Analytics identified a member who was taking the name brand Sabril while a cost saving generic called vigabatrin was available. The HighTouchRx team contacted the prescriber and recommended the member switch to the generic vigabatrin, which resulted in savings for the health plan and the member. Switching to this generic has saved health plans over $200,000 annually and members roughly $360.
Optimizing Hemilbra® regimen: HighTouchRx gathered recent weight data from a member taking Hemilbra, and the team recommended reducing number of vials a provider billed. The result was significant health plan savings with no out-of-pocket impact for the member. HighTouchRx simplified the regimen and saved the health plan $168,000 annually.
PreserveRx provides protection from financial risks7
PreserveRx is an excess reinsurance product with configurable attachment points for health plans. It covers gene therapies at 100% of wholesale acquisition cost (WAC). Pricing is set at a per member per month premium. PreserveRx seeks to protect both health plans and employers from sudden, one-time costs due to covering ultra-expensive gene therapies, while preserving access to these potentially life-changing or curative gene therapies for members. This clinical and financial solution is specifically designed to reinsure high-cost gene therapies for payers that cover these gene therapies and help preserve member access and coverage for these life-altering therapies.
Portable patient registries: Where the payment follows the patient:
Portable patient registries are inventories of particular resource utilization at a point in time, that are independent from a single health plan insurer. For example, Joe Smith has his CAR-T treatment while insured by Blue Plan X, who begins four years of payments to the manufacturer. Two years later, Joe gets a new job and is insured by Blue Plan Y. The CAR-T contract follows Joe to Blue Plan Y and Blue Plan Y begins the final two years of payments to the manufacturer.6
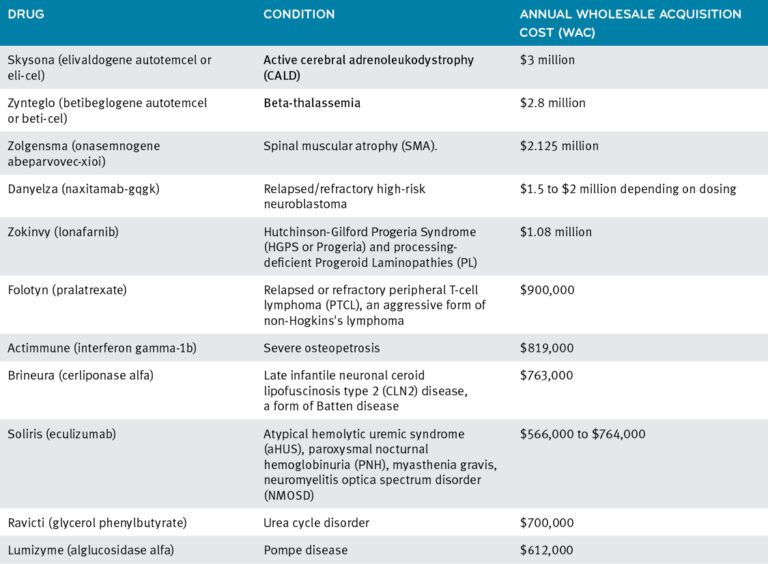
10 of the Most Expensive Drugs in the US8
References
- Bowen K, Starner C, Gleason P. 2016 to 2019 Trend in Integrated Total Pharmacy Plus Medical Benefit Drug Spend—Doubling of Members with Extremely High Annual Drug Cost within a 17 Million Commercially Insured Population. Academy of Managed Care Pharmacy virtual national conference. October 2020. Accessed at: https://www.primetherapeutics.com/content/dam/corporate/Documents/Newsroom/Pressreleases/2019/document-amcpposter-superspenders.pdf
- Bowen K, Gleason P. Drug Super Spenders: 2016-2018 Growth in Number of Members and Total Pharmacy Plus Medical Benefit Drug Cost for Members with Extremely High Annual Drug Cost in a 17 Million Member Commercially Insured Population. Academy of Managed Care Pharmacy national meeting Baltimore, MD. October 2019. J Manag Care Spec Pharm 2019:25(10-a):S90. https://www.jmcp.org/doi/pdf/10.18553/jmcp.2019.25.10-a.s1
- Shamard Charles, M.D. No end in sight to rising drug prices, study finds. May 13, 2019. NBC News. Accessed at: https://www.nbcnews.com/health/health-care/no-end-sight-rising-drug-prices-study-finds-n1012181
- Maas, Angela. Prime Therapeutics launches IntegratedRx – Oncology, partners on MIP Accreditation. Nov. 16, 2021. As published in Radar on Specialty Pharmacy. Accessed at: https://www.primetherapeutics.com/news/prime-therapeutics-launches-integratedrx-oncology-partners-on-mip-accreditation/
- Sahli, Brett. Cost management for sky-high, high-cost gene therapy. August 17, 2021. © Prime Therapeutics Inc. Accessed at: https://www.primetherapeutics.com/news/cost-management-for-sky-high-high-cost-gene-therapy/
- Myshko, Denise. Prime Develops Predictive Model to Identify Savings in Breast Cancer. Sept. 7, 2022. Formulary Watch. Accessed at https://www.formularywatch.com/view/prime-develops-predictive-model-to-identify-savings-in-breast-cancer
- Three Minutes with Patrick Gleason – Prime Therapeutics LLC. Feb. 7, 2022. Prime News Perspectives. ©Prime Therapeutics.com. Accessed at: https://www.primetherapeutics.com/news/three-minutes-with-patrick-gleason/
- 10 of the Most Expensive Drugs in the US. Oct 17, 2022. Drugs.com. Accessed at: https://www.drugs.com/slideshow/top-10-most-expensive-drugs-1274
Related news
Perspectives
July 25, 2024
Quarterly Drug Pipeline: July 2024
Clinical insights and competitive intelligence on anticipated drugs in development
Perspectives
July 22, 2024
Oncology Insights: 2024 ASCO Annual Meeting key findings
Findings from this year’s American Society of Clinical Oncology (ASCO) Annual Meeting will likely lead to clinical practice changes and U.S. Food and Drug Administration (FDA) drug approvals or expansions
Perspectives
July 16, 2024
LISTEN NOW: Beyond the business – Stories of corporate kindness | Pharmacy Friends Podcast
In this episode, we talk about how our employees' help goes beyond our work in health care, aiding in philanthropic efforts