Perspectives
Study of short-acting, long-acting and abuse-deterrent opioid use
The mix of opioids is crucial to the cost impact of abuse-deterrent opioids
November 30, 2017What was the study about?
With opioid use and abuse continuing to rise, plan sponsors need to use every tool at their disposal. Prime continues to identify valuable insights from years of pharmacy and medical analysis expertise.
This study looked at medical and pharmacy claims to define and divide utilization patterns, quantities, dosages and diagnoses into three separate groups:
- Members who were only prescribed short-acting opioids
- Members who were only prescribed long-acting opioids
- Members who were prescribed both short- and long-acting opioids
What did we learn?
Most members who get opioids are prescribed short-acting opioids. And most of them have only one or two claims. That is consistent with prescribing guidelines.
But groups of members exist that appear to be experiencing non-typical opioid prescribing. This gives a plan sponsor thousands of members where they might intervene to improve health outcomes and increase savings.
Methods
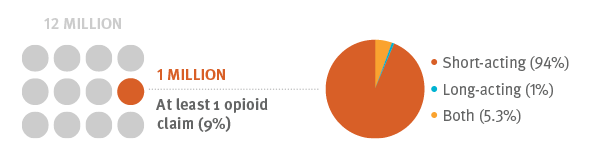
We identified more than 1 million members (9 percent) who had at least one opioid claim (out of 12 million continuously enrolled from July 1, 2013 to Sept. 1, 2014). These members were divided into the three groups identified above. The groups were followed for 12 months. Medical claims were used to further divide them by diagnosis.
Results
Short-acting only: 94 percent (of the 9 percent) were prescribed short-acting opioids. As would be expected, nearly two thirds of these members received only one or two prescriptions. 66 percent of members received only one prescription with less than 10 pills. But 6 percent of members had 16 or more claims within 12 months. This indicates the use of short-acting opioids for long-term chronic opioid therapy.
Long-acting: Only 1 percent (of the 1 million opioid utilizers) were prescribed long-acting opioids. Just over half of these members received only one or two prescriptions. 62 percent of these members were new starts – they had no claims for opioids in the previous 120 days. It is unsafe to initiate opioid therapy with a long-acting opioid. The CDC recommends against it. 9 percent of these members had 16 or more claims within 12 months. These members are on chronic opioid therapy with only long-acting opioids. Long-acting opioid therapy should always include a short-acting opioid for break through pain. It is not recommended to be on long-acting opioid therapy only. These all represent opportunities for interventions.
Short- and long-acting: 6 percent (of the 1 million) were prescribed both short- and long-acting opioids. 54 percent of these members had 16 or more claims within 12 months. 4 percent of these members had a cancer diagnosis.
Diagnoses: Most common diagnoses for all three groups were: low back pain, joint pain and arthritis, followed by abdominal pain and headache. Percentages varied for each. The study poster includes more detail. The CDC recommends avoiding opioids for the treatment of back pain and headache.
Conclusions
GuidedHealth® interventions can target:
- Long-acting opioid utilizers
- Members with a large quantity of opioids in a short period of time
- Members without evidence of diagnosis
- A prior authorization (PA) program could help address opioid use patterns among large numbers of new starts. Potential savings for a new start PA could save $0.01 per member per month.
Additional research could focus on short- vs long-term use, and concurrent treatments – like use of benzodiazepines and opioid prescriptions.
What does this mean for you?
Prime’s Controlled Substance Management Program can help plan sponsors identify members with a variety of risk profiles, using specific claim analyses and predictive models. A range of clinical and outreach programs are available to help plan sponsors achieve savings, quality and outcomes goals.
Related news
Perspectives
April 17, 2024
AMCP 2024: Behind the research with YuQian Liu
Ahead of her session with Andy Killpack, Liu — senior director of specialty clinical solutions at Prime/MRx — shares current care management strategies for cell and gene therapy and the future of this exciting frontier
Perspectives
April 16, 2024
AMCP 2024: Behind the research with Jacob LaRue and Timothy O’Shea
Ahead of their session, Jacob and Timothy share how Prime/MRx is working alongside providers like Horizon Blue Cross Blue Shield of New Jersey to manage drug waste and rein in spend for specialty drugs without therapeutic impact to patients
Perspectives
April 15, 2024
Oncology Insights: Cancer treatment is personal
Precision medicine, or personalized medicine, uses genes or proteins to diagnose or treat disease. This medical care design has significantly impacted oncology and grew out of a need to improve and individualize patient treatments