Perspectives
Never again should you doubt the power of benefit design
A point of sale edit at the pharmacy shortened opioid prescriptions to less than seven days supply
February 20, 2020Opioids are often prescribed for relief of acute pain, like following an injury or outpatient surgery. Evidence shows that (most of the time) a three-day opioid prescription will be sufficient. Industry experts from the Centers for Disease Control (2016) have provided these guidelines.¹ Many states have passed laws supporting these guidelines.²
As these guidelines have become more well known, doctors started to change their opioid prescribing behaviors. Fewer long prescriptions. More prescriptions for less than a week.
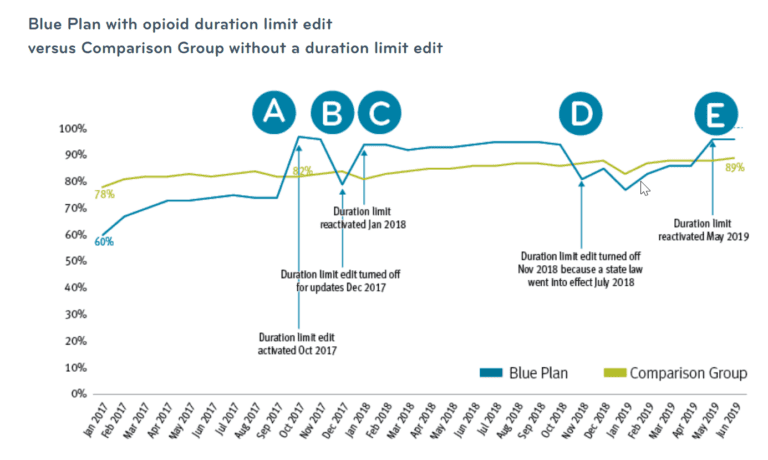
By 2018, several of Prime’s Blue Plan clients were filling more than 80 percent of opioid prescriptions as less than seven day supply. One Blue Plan, however, had a much lower rate. Could a change in benefit design improve the number of less than seven day supply opioid prescriptions?
Yes. A point of sale edit made the difference.
This Blue Plan implemented a duration limit editA for members new to opioid therapy – no opioid claims in members history for 180 days. The edit required longer opioid prescriptions to be filled for less than seven days’ supply. The number of patients new to opioid therapy who received less than a seven day supply increased to 97 percent.
Two months after it started, the duration limit edit was briefly turned off for some administrative updates. The rate dropped 18 points very quickly.B But when it was turned back on, the rate bounced right back up.C Then, the Blue Plan rate held in the mid 90th percentile for most of the next year.
State law vs point of sale edit.
This Blue Plan client also learned the difference in effectiveness between a point of sale edit and state law.
In 2018, that state government passed a law requiring shorter opioid prescriptions for members new to opioids. The Blue Plan decided to turn off the point of sale edit.D Wouldn’t the state law accomplish the same objective?
No, it didn’t. The percentage of short day supply opioid prescriptions dropped back into the 70s again.
So, a few months later the Blue Plan put the edit back into place. The short days supply rate bounced back up into the mid 90s again.E
Your PBM knows pharmacy benefits
From start to finish of the 2.5 year study, the percentage of members with a less than seven day opioid prescription increased 36 percent, from 60 percent to 96 percent. The comparison group percent of short day supply opioid prescriptions only increased 11 percent.
These findings are one small part of the research parsed from 30 months of pharmacy claims data studying a 2 million member group with a 1.6 million member comparison group.
Many benefit designs support controlled substance management
This point of sale edit is just one example of many Prime offerings that help health plans control potential opioid misuse and abuse. Learn more about Prime’s commitment to controlled substance management.
References
1. Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. JAMA. 2016;315(15):1624.
2. National Conference of State Legislators. Prescribing Policies: States Confront Opioid Overdose Epidemic. NCSL website. http://www.ncsl.org/research/health/prescribing-policies-states-confront-opioid-overdose-epidemic.aspx. Published October 31, 2018. Accessed January 10, 2019.
Related news
Perspectives
April 19, 2024
LISTEN NOW: Live at AMCP Annual 2024 – Digging into managed care pharmacy insights | Pharmacy Friends podcast
In this episode, Prime/MRx clinicians — along with special guests — discuss the hottest topics covered at the Academy of Managed Care Pharmacy (AMCP)'s 2024 Annual Meeting in New Orleans
Perspectives
April 17, 2024
AMCP 2024: Behind the research with YuQian Liu
Ahead of her session with Andy Killpack, Liu — senior director of specialty clinical solutions at Prime/MRx — shares current care management strategies for cell and gene therapy and the future of this exciting frontier
Perspectives
April 16, 2024
AMCP 2024: Behind the research with Jacob LaRue and Timothy O’Shea
Ahead of their session, Jacob and Timothy share how Prime/MRx is working alongside providers like Horizon Blue Cross Blue Shield of New Jersey to manage drug waste and rein in spend for specialty drugs without therapeutic impact to patients