Perspectives
Mind the gap: Using a drug’s price-to-value calculation
This price is based on the value a drug can deliver to a patient’s life.
December 19, 2019“Is it worth that much?”
That question might be heard in a department store, by someone weighing a decision about buying a new pair of shoes.
But is it a question someone might ask about a prescription drug? Yes. And Prime does.
Rising prescription drug costs have been a major driver of rising health care costs. When combined, pharmacy and medical drugs make up 30 percent of health care costs. And six- and seven-figure drug treatments are launching on a regular basis.
To help beat back rising and unsustainable drug prices, we’re factoring in new elements such as QALY (quality-adjusted life year) and price-to-value frameworks into drug price analysis.
It can be helpful to have a little more background about these related terms, since together, they play a growing role in being able to push back on manufacturers’ high drug costs. Manufacturers are paying attention; many have dropped prices in response to these value assessments.1,2,3
One QALY equals one year in perfect health
QALY stands for quality-adjusted life year. Think of QALY as an analysis that combines quality of life and life expectancy. It’s not new. But QALY has become more commonly used in the past ten years, helped considerably by protocols developed by ICER (Institute for Clinical and Economic Review), a key national, nonprofit research organization that publishes pricing evaluations on drugs and drug classes.
This is from ICER’s website: “The quality-adjusted life year (QALY) is the gold standard for measuring how well a medical treatment improves and lengthens patients’ lives, and therefore has served as a fundamental component of cost-effective analyses in the United States and around the world for more than 30 years.”4,5
Organizations have grown to accept QALY as part of the equation they use to assess the value of drugs compared to prices.
Here’s how it works: A 50-year-old woman, in general, has a life expectancy of another 35 years. If she is healthy, those 35 years might all count as 35 QALYs.
If that 50-year-old woman has multiple sclerosis (MS), however, she has compromised health. She might need daily help and have less mobility over time. Researchers may adjust those 35 years down by 15 QALYs.
When a new drug’s clinical research is published, ICER uses a careful, methodical process to convert the outcomes into QALYs.
Multiply the extra QALYs by $150,000, a predetermined cost per QALY
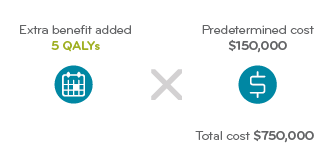 ICER’s calculations may determine that this new drug contributes five QALYs to the patient’s life. (ICER has a helpful report that explains its system.9)
ICER’s calculations may determine that this new drug contributes five QALYs to the patient’s life. (ICER has a helpful report that explains its system.9)
ICER uses a range of $50,000 to $150,000 to quantify the value of one year of good health. This seems like a fair investment because the median household income in the United States is $50,000 per year.
For purposes of this illustration, let’s say ICER’s analysis suggests the new drug will add five QALYs to the patient’s life. Five QALYs times $150,000 per year is $750,000.
Divide by the number of years the drug will be used, in this case 35.
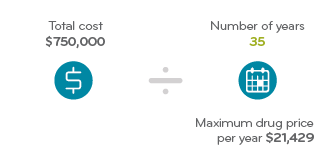 The woman may live another 35 years, so the QALY total of $750,000 is divided across that entire time period. That comes to $21,429 per calendar year. Using ICER’s methodology, this is what they determine to be the annual value of the drug.
The woman may live another 35 years, so the QALY total of $750,000 is divided across that entire time period. That comes to $21,429 per calendar year. Using ICER’s methodology, this is what they determine to be the annual value of the drug.
Said another way, the annual price of this hypothetical MS drug, which adds five QALYs, should be set at no more than $21,429.
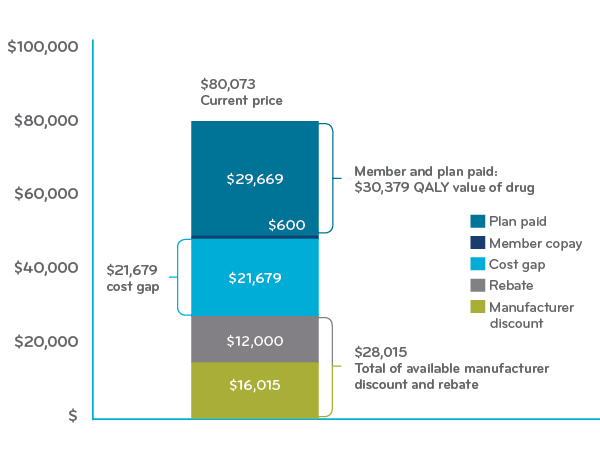
Next, we’ll look at how value shows up in a price-to-value framework. (Note: The chart below uses a different pricing example.)
Breaking down price to value for disease-modifying drugs
MS is an example of an expensive specialty condition with a growing annual cost. More than 400,000 people in the United States (and perhaps more) have MS. Treatment breakthroughs can now help people avoid relapses, slow the disease’s progression and improve their quality of life.6
This chart below represents a blend of disease-modifying drugs (DMDs) used to treat MS. The average annual cost for the DMDs was $80,073.
To find the price-to-value cost gap, take that figure minus:
- ICER’s suggested price of $30,379 (paid by the member and health plan), and
- $28,015 paid through manufacturer discounts and rebates
That leaves $21,679 as the average price-to-value cost gap for DMD drugs.
Multiple sclerosis DMD Self-administered average annual actual cost (ICER 2017 Report)
Big conversations are required to move the dial on this
ICER and many other studies have concluded that the price of MS DMDs greatly exceeds conventional thresholds for cost-effectiveness. The following table from ICER shows the percentage reductions needed in the prices of these drugs to bring them in line with the value of these drugs.7,8
Value-based price benchmarks for pharmacy benefit obtained by MS disease modifying therapies (DMTs)10
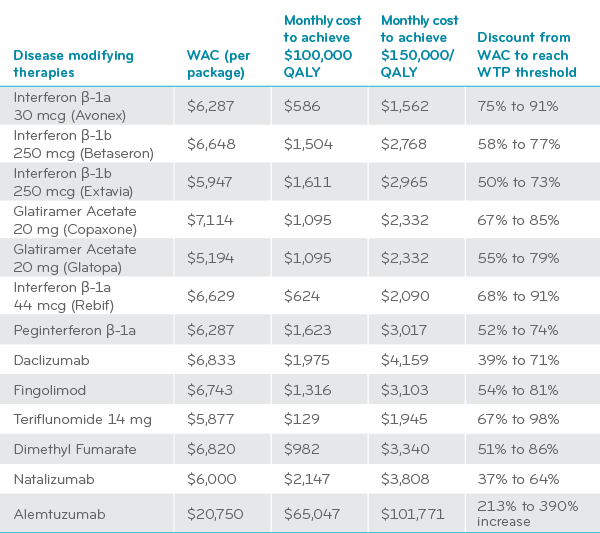
WAC = wholesale acquisition cost WTP = willingness to pay threshold
Prime is a member of ICER and is working with prestigious nonprofit research organizations like ICER and ISPOR (International Society for Pharmacoeconomics and Outcomes Research). They are publishing value frameworks for high cost drugs and it’s changing the dialogue in the marketplace.11-12 Prime is at the table.13 But there is still more to do.
References
- “Can ICER bring cost effectiveness to drug prices?” by Lola Butcher. May 28, 2019. Managed Care. Accessed at: https://www.managedcaremag.com/archives/2019/6/can-icer-bring-cost-effectiveness-drug-prices
- “With new report, ICER puts itself at center of drug pricing storm,” by Ned Pagliarulo, Oct. 8 2019. BioPharmaDrive. Accessed at: https://www.biopharmadive.com/news/icer-unsupported-drug-price-increases-pharma/564539/
- The QALY: Rewarding the Care That Most Improves Patients’ Lives. ICER. December 2018. Accessed at: https://icer-review.org/material/the-qaly-rewarding-the-care-that-most-improves-patients-lives/
- “Obscure Model Puts a Price on Good Health—and Drives Down Drug Costs,” By Denise Roland. Nov. 4, 2019. Wall Street Journal. Accessed at: https://www.wsj.com/articles/obscure-model-puts-a-price-on-good-healthand-drives-down-drug-costs-11572885123?mod=hp_lead_pos5
- “Quantifying life: Understanding the history of Quality-Adjusted Life-Years (QALYs),” by Eleanor MacKillop and Sally Sheard. Social Science and Medicine. 2018 Aug; 211: 359–366. doi: 10.1016/j.socscimed.2018.07.004. Accessed at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6079188/
- https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Brochure-History-of-Multiple-Sclerosis.pdf
- Institute for Clinical and Economic Review (ICER). Summary report: https://icer-review.org/wp-content/uploads/2017/03/CTAF_MS_RAAG_030617.pdf, accessed on Jan 19, 2018
- Institute for Clinical and Economic Review (ICER). MS Final report: Accessed at: https://icer-review.org/wp-content/uploads/2016/08/CTAF_MS_Final_Report_030617.pdf
- ICER Value Assessment Framework, ICER. Accessed at: https://icer-review.org/methodology/icers-methods/icer-value-assessment-framework-2/
- Disease-Modifying Therapies for Relapsing Remitting and Primary-Progressive Multiple Sclerosis: Effectiveness and Value: Final Evidence Report, March 6, 2017. Figure 28, page 87. ICER. Accessed at: https://icer-review.org/material/ms-final-report/
- Pearson SD, Thokala P, Stevenson M, Rind D.The Effectiveness and Value of Treatments for Spinal Muscular Atrophy. J Manag Care Spec Pharm. 2019 Dec;25(12):1300-1306. https://www.jmcp.org/doi/10.18553/jmcp.2019.25.12.1300
- Starner CI, Gleason PP. Spinal Muscular Atrophy Therapies: ICER Grounds the Price to Value Conversation in Facts. J Manag Care Spec Pharm. 2019 Dec;25(12):1306-1308. https://www.jmcp.org/doi/full/10.18553/jmcp.2019.25.12.1306
- Willke RJ, Chapman RH, Seidman JJ, Schnipper LE, Gleason PP. Current Value Frameworks-What’s New? Value Health. 2019 Jun;22(6S):S7-S11. doi: 10.1016/j.jval.2019.04.1916.
Related news
Perspectives
April 25, 2024
Drug Approvals Monthly Update: April 2024
This monthly update of United States (U.S.) Food and Drug Administration (FDA) approvals…
Perspectives
April 24, 2024
Prime/MRx resident wins AMCP Foundation Best Poster Award
Ai Quynh Nguyen, PharmD, was recently recognized for her research on opioid-prescribing patterns and outcomes
Perspectives
April 23, 2024
Expert Clinical Network Insights: April 2024
A look into our Expert Clinical Network (ECN) – part of Prime/MRx’s value-based approach to medical and pharmacy benefit management that offers access to more than 175 national and world-renowned key opinion leaders in multiple disease categories who provide expertise on challenging prior authorization case reviews, peer-to-peer discussions, drug policy development and formulary guidance